Left atrial minimum volume index (LAVImin) as measured by cardiac MRI is useful for predicting future major adverse cardiovascular events (MACE) after acute myocardial infarction (AMI), according to research published September 16 in Radiology.
The findings support LAVImin as an independent prognostic biomarker and using cardiac MRI instead of echocardiography for risk stratification, according to Jingping Wu, MD; Jinyi Xiang, MD; and colleagues from Shanghai Jiao Tong University in China.
"Our research, involving a large cohort of participants with AMI, provides compelling evidence that supports the integration of LAVImin into clinical evaluation," the group wrote. "Importantly, doing so does not require additional scanning time, as LAVImin can be calculated using cine images that are already acquired in standard cardiac MRI protocols."
The left atrium plays a key role in regulating blood volume and blood pressure, and LAVI is a critical value in the diastolic evaluation algorithm outlined in current guidelines; however, the algorithm emphasizes LAVI maximum (LAVImax) volume, the group explained. Less is known about LAVImin derived from cardiac MRI in patients with AMI and its incremental prognostic value beyond established markers.
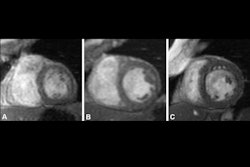
To bridge the gap, this study involved 1,191 patients (mostly men; median age, 58) with AMI, who underwent percutaneous coronary intervention within 12 hours and a cardiac MRI exam within seven days from symptom onset. Scans, including late gadolinium enhancement imaging, were obtained on two 3-tesla platforms from different vendors (Siemens and Philips) and postprocessed using dedicated software (cvi42; Circle Cardiovascular Imaging).
About 15% of participants (183) experienced MACE within 14 months. Participants with LAVImin greater than the optimal cutoff 18.74 mL/m2 showed an increased risk of each MACE outcome, Wu, Xiang, and colleagues reported, among other cardiac MRI parameters and correlations.
LAVImin remained an independent predictor of MACE, the group noted. LAVImin had better discriminative ability for MACE than LAVImax, with an area under the receiver operating characteristic curve (AUC) of 0.74, compared with 0.65; p < 0.001, and LA conduit strain (AUC, 0.64; p < 0.001).
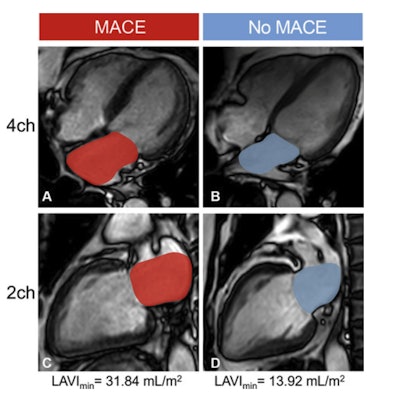 Cardiac MRI cine images in the (A, B) four-chamber (4ch) and (C, D) two-chamber (2ch) views illustrate contouring (red and blue areas) for measurement of left atrial (LA) minimum volume index (LAVImin) at end diastole in two representative participants with acute myocardial infarction (AMI). The LA appendage and pulmonary veins were not considered part of the LA volume. (A, C) Images in a 76-year-old man with a history of coronary artery disease who underwent contrast-enhanced cardiac MRI 4 days after AMI and experienced a major adverse cardiovascular event (MACE), in this case death, during follow-up. LAVImin was 31.84 mL/m2 in this participant. (B, D) Images in a 38-year-old man with a history of angina who underwent contrast-enhanced cardiac MRI 4 days after AMI and did not experience MACE during follow-up. LAVImin was 13.92 mL/m2 in this participant.Caption and image courtesy of RSNA.
Cardiac MRI cine images in the (A, B) four-chamber (4ch) and (C, D) two-chamber (2ch) views illustrate contouring (red and blue areas) for measurement of left atrial (LA) minimum volume index (LAVImin) at end diastole in two representative participants with acute myocardial infarction (AMI). The LA appendage and pulmonary veins were not considered part of the LA volume. (A, C) Images in a 76-year-old man with a history of coronary artery disease who underwent contrast-enhanced cardiac MRI 4 days after AMI and experienced a major adverse cardiovascular event (MACE), in this case death, during follow-up. LAVImin was 31.84 mL/m2 in this participant. (B, D) Images in a 38-year-old man with a history of angina who underwent contrast-enhanced cardiac MRI 4 days after AMI and did not experience MACE during follow-up. LAVImin was 13.92 mL/m2 in this participant.Caption and image courtesy of RSNA.
Incorporating LAVImin into post-AMI assessments could support targeted interventions and improve outcomes, especially in patients with established risk factors such as diabetes, elevated Killip class, or reduced ejection fraction, Wu, Xiang, and colleagues added.
In an accompanying editorial, Jonathan Weir-McCall, PhD, and Alina Hua, PhD, of King’s College London and Royal Brompton Hospital in the U.K. said that while a strong and independent prognostic link has been established for LAVImin, the question remains as to how to address this risk.
"If it is indeed a marker of increased end-diastolic pressure, this would usefully highlight a cohort in the greatest need of medications that target this, such as angiotensin-converting enzyme inhibitors, angiotensin receptor blockades, and beta-blockers," Weir-McCall and Hua wrote. "Alternatively, an increased LAVImin may reflect greater LA fibrosis and stiffening, for which there are currently no medications."
Understanding through which of these pathways the risk is mediated will be critical to determine whether LAVImin should become a standard cardiac MRI reporting metric in patients after acute myocardial infarction and how it should be managed, Weir-McCall and Hua said.
See all metrics and read the complete paper here.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











