There are a number of options for lung nodule imaging, and which to use depends on the patient, according to a talk delivered April 30 at the American Roentgen Ray Society (ARRS) meeting in San Diego.
"[For lung imaging] we have to think about our diagnostic strategy," presenter Hiram Shaish, MD, of Columbia University Medical Center in New York City, told session attendees. "We have to think about the patient in front of us. If we're looking at a 12-year-old who has a cough and fever and a lung nodule on x-ray, we're not going to recommend a CT but rather follow-up, whereas an older, smoking adult would be in a different risk category."
Shaish outlined the benefits of different imaging modalities and technique for identifying and characterizing lung nodules.
CT
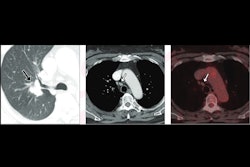
CT is the "mainstay" for characterizing pulmonary nodules, Shaish noted. These exams are conducted with or without contrast, and they can provide information on nodules' shape, size, density, calcification, location, and morphology (ground glass, part solid, oval solid, solid). They also help clinicians assess nodules' margins -- smooth, lobulated, and spiculated.
CT can also help determine the density of a nodule, which is "not something we always think about," Shaish said, but "a very dense nodule is associated with benign behavior."
Tracking a nodule's growth rate is key, according to Shaish. He noted that a nodule's diameter increases by 26% with a doubling of volume, and that CT doubling times range from 79 to 1,435 days (mean, 508 days).
"[Monitoring growth rate] is one of the few things we can do as radiologists quite accurately that can clue us in about what the nodule is actually doing," he said.
MRI
Lung nodules can be detected on MRI using a short tau inversion recovery (STIR) turbo spin-echo (SE) or half-Fourier acquisition single-shot turbo spin-echo (HASTE) with black-blood technique and respiratory gating protocol -- or using a thin-section MR imaging with ultrashort echo time (TE) and respiratory gating, Shaish said.
He described MRI protocols that can characterize lung nodules:
• T1-weighted turbo SE or HASTE with black-blood technique
• 3D T1-weighted spoiled gradient echo (GRE) sequence with fat suppression
• T2-weighted turbo SE or HASTE with black-blood technique;
• STIR turbo SE or HASTE
• Diffusion-weighted imaging to assess apparent diffusion coefficient (ADC) and lesion-to-spinal cord ratio
• Contrast-enhanced T1 and 3D spoiled GRE
"MRI's strength [for lung imaging] is its ability to distinguish soft tissues from each other," Shaish noted.
F-18 FDG-PET/CT
When it comes to characterizing lung nodules using PET/CT, clinicians can look for the following results:
• A high standardized uptake value (SUV) -- more than 2.5 -- suggests malignancy.
• Low/no uptake suggests that the nodule is benign.
• Intense, irregular uptake suggests higher suspicion of malignancy.
PET/CT's advantages for lung nodule imaging include a high sensitivity for malignancy (85% to 95%) and an ability to detect hidden metastases. Its downsides include false positives or negatives, Shaish said.
Radiomics
Finally, radiomics can help distinguish benign from malignant nodules, predict disease outcomes, and monitor treatment response through flagging imaging biomarkers, Shaish noted.
"We're talking about harnessing the data inside the images that human eyes don't perceive," he concluded.