Digital breast tomosynthesis (DBT) has its advantages over conventional mammography in women with a family history of breast cancer, suggest findings published in JAMA Oncology.
DBT screening reduced recall rates and increased specificity compared to digital mammography in a study led by Tong Li, PhD, from the University of Sydney in Australia and colleagues.
“Breast radiologists could use this information to recommend DBT to women with a family history of breast cancer," Li told AuntMinnie.com. "This may help reduce patient anxiety and avoid unnecessary procedures without compromising cancer detection."
Family history of breast cancer is a well-established risk factor for the disease, and women in this patient population are more likely to have dense breasts. DBT, meanwhile, has shown promise in previous studies for reducing recall and detecting more cancers, especially in young women.
Li et al compared the performance of DBT and digital mammography screening in women with a family history of breast cancer overall. It also subdivided women by breast cancer family history category, breast density, age group, screening interval, and screening round. Finally, the team described characteristics of cancers detected on screening versus interval cancers. The women were imaged facilities affiliated with the Breast Cancer Surveillance Consortium.
The study included 208,945 women with a family history of breast cancer. The women underwent a total of 502,357 screening exams.
Adjusted absolute risk differences (ARDs) when comparing DBT versus mammography were significant for recall rate (-1.51%) and specificity (1.56%) in the overall cohort. This trend continued for women with one first-degree relative, with a recall rate ARD of -1.72 and a specificity ARD of 1.75%. Women with only second-degree relatives who underwent DBT had a significantly higher biopsy rate compared to the mammography group (ARD, 0.39%).
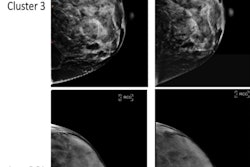
The team also reported significant ARDs for ductal carcinoma in situs (DCIS) detection rate at -0.71 per 1,000 exams in women with almost entirely fatty breasts. ARDS for recall rate and specificity for women with scattered fibroglandular densities were -1.9% and 1.93%, respectively.
The researchers also found significant ARDs for the following: positive predictive value for recall (1.75%) in heterogeneously dense breasts, biopsy rate (0.48%), and advanced cancer rate (-0.61 per 1,000 exams) in extremely dense breasts.
Finally, the team highlighted that DBT screening had a higher proportion of screen-detected early-stage, invasive cancers with favorable prognostic features.
Li said that these findings suggest that screening with DBT may result in fewer harms than digital mammography for women with a family history of breast cancer.
"The study also highlights the need to consider breast density and screening interval when selecting imaging modalities," she said. "While not definitive, the evidence adds support for more tailored screening approaches in this group of women."
Li told AuntMinnie.com that the team future research could help clarify how DBT can be most effectively used in these women.
"It could be valuable to explore how screening guidelines could be adjusted based on the number or degree of affected relatives and breast density," she said. "There is also a need to examine how factors like age, screening history, and breast density might guide more personalized screening approaches."
The full study can be read here.