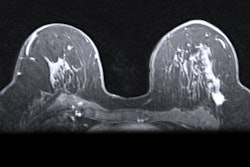
Undergoing regular breast cancer screening starting at age 40 leads to better health outcomes for women, according to research published May 30 in Radiology: Imaging Cancer.
A team led by Jean Seely, MD, from the University of Ottawa in Canada found that compared with symptomatic breast cancers, screen-detected cancers in women age 40 or older led to lower odds of advanced cancer, mastectomy, and breast cancer-related death.
“Breast radiologists can use this information to encourage their patients to have early detection of breast cancer through screening before symptoms of breast cancer develop,” Seely told AuntMinnie. “Radiologists should track the method of breast cancer detection to show the positive benefits of early detection.”
The debate continues on whether women should start being screened for breast cancer at age 40 versus age 50. Imaging societies say women of average lifetime risk should attend their annual mammography appointments. The U.S. Preventive Services Task Force (USPSTF), meanwhile, changed its breast screening recommendations from starting biennial screening at 50 years old to 40, a B-grade recommendation. Women aged 75 and older, however, are still not recommended for regular screening, per USPSTF guidelines.
Seely and colleagues investigated the impact of how breast cancers are found on disease staging, treatment, and breast cancer-related mortality in women aged 40 or older. The retrospective study included data collected in 2016 from 821 women with an average age of 62.5 years and an average follow-up duration of 6.7 years.
In less-screened groups, including women ages 40 to 49 and women at 75 and older, the team reported more frequency of symptom-detected cancers (72.9% and 70.4%, respectively). Screened age groups had less frequency of symptom-detected cancers at 49.5% (women ages 50 to 59) and 33.3% (women ages 60 to 74), respectively.
Compared with symptom-detected cancers, screen-detected cancers had a 6.6-times greater odds of lower tumor staging (p < 0.001) after adjustment for age at diagnosis. Of the 821 advanced cancers included in the study, 10.2% were screen-detected (n = 84) and 32.5% were symptom-detected (n = 267).
Symptom-detected cancers had a hazard ratio of 1.63 for breast cancer-related death (HR, 1.63; p = 0.004) and higher odds of mastectomy (odds ratio [OR], 2.20; p < 0.001) compared to screen-detected breast cancers. The team also reported similar odds of chemotherapy for both detection methods, even after adjustment for age and stage at diagnosis.
Finally, multivariable analysis showed significant ties between higher tumor stage and the following factors: symptom detection (OR, 6.40; p < 0.001), greater risk of chemotherapy (OR, 1.97; p < 0.001), and age at diagnosis (OR, 1.02; p = 0.001).
Seely said that breast cancer screening should start at age 40 with these results in mind, and that screening should continue for women who are older than 74 and in good health.
“We did not look at screening frequency in our study, but women who were screen-detected attended every one to two years, depending on their risk factors,” Seely said. “Regular screening every one to two years for women ages 40 years and older is recommended.”
She told AuntMinnie.com the team is currently studying women who were diagnosed with breast cancer in the province of Ontario. The goal is to compare outcomes of mortality, including all-cause and breast cancer-specific, at 10 years and stage at detection, according to their method of detection.
“We are also studying the benefits of adding AI to screening mammography and optimizing the selection of women who will benefit from supplemental screening due to risk factors and those with dense breast tissue to ensure they also benefit from screen-detection of breast cancer,” Seely said.
The study can be read in its entirety here.