While contrast-enhanced ultrasound (CEUS)'s growth in clinical use has been modest, sonography experts say there is reason for optimism for the technique.
The International Contrast Ultrasound Society (ICUS) recently urged the Centers for Medicare and Medicaid Services (CMS) to adjust codes assigned for certain CEUS exams.
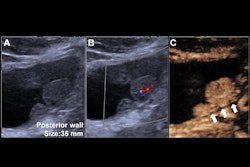
“We’ve been using ultrasound contrast for more than 20 years,” said Richard Barr, MD, of Northeast Ohio Medical University in Rootstown and an officer at ICUS. “Our urologists don’t [choose] CT and MR [exams] for renal mass evaluations anymore because there are errors.”
The ICUS’ letter to the CMS calls for the reassignment of current procedural terminology (CPT) codes 76978 and 76979, which cover noncardiac CEUS scans, to APC 5572, which stands for level two imaging with contrast. ICUS, however, is not seeking a change in reimbursement for cardiac CEUS.
The society stated that reassigning these CPT codes will align reimbursement with the clinical and economic benefits of CEUS.
Richard Barr, MD, discusses how higher reimbursement can help grow the use of CEUS in imaging practices.
The first federally approved microbubble contrast agents appeared in the U.S. in the late ‘90s, though the concept can be traced back to the ‘60s. Researchers first used CEUS in echocardiography to improve low-quality imaging studies. Despite much research into CEUS’ broader use, it wasn’t until 2016 that the U.S. Food and Drug Administration (FDA) approved the first microbubble-based contrast agent for noncardiac use. This included approvals for imaging of the liver and pediatric urinary tract for Lumason.
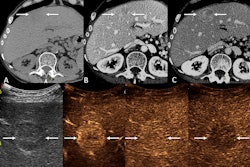
The echogenic nature of microbubbles in these agents improves ultrasound images via a strong signal-to-noise ratio and high temporal resolution that helps with imaging for blood vessels and soft tissue. CEUS proponents say the technique has advantages over other contrast imaging methods, including CT and MR exams that use gadolinium and iodine. As well, recent studies suggest that CEUS is effective in procedures such as ablation and biopsy.
Proponents also highlight that microbubble agents are safer since they have no effect on organ function, do not impart radiation, and are more easily accessible than those needed for CT or MRI exams. While microbubble contrast agents may cause allergic reactions in some patients, research suggests that these cases are rare and mostly mild.
“It’s probably the safest of the contrast agents for abdominal imaging,” said Barr, who is also a fellow at the American Institute of Ultrasound in Medicine (AIUM) and serves as editor-in-chief of the Journal of Ultrasound in Medicine. “We can use it in patients with renal failure and in pregnant patients. And these patients often have problems that we can’t solve without a contrast agent.”
Barr added that CEUS can also improve patient care by improving time to diagnosis, explaining that most exams can be read within the same day with no further testing. In fact, survey study results presented September 10 at the ICUS Bubble Conference in Chicago suggested that CEUS helps streamline hospital workflows, with respondents stating that the exam does not require sedation, anesthesia, or the need to transport patients to larger scanners.
A study published in 2018 found that a metropolitan-area hospital saved about $117,000 annually by using CEUS in the initial scanning of liver and kidney lesions without waiting for further CT or MRI procedures.
Experts have noted that despite the evidence of the modality’s efficacy and safety profile, CEUS’ growth has not been as big as was hoped. Barr said that while CEUS’ use in the pediatric and interventional specialties has experienced significant growth, its use in general imaging has not.
Cynthia Peterson from Kent State University in Portage County, OH, said that the COVID-19 pandemic played a part in slowing progress for CEUS’ growth.
“Anything that was extra or new had to be tabled, so patients could receive the care they needed,” said Peterson, who is also a member of the Society of Diagnostic Medical Sonography (SDMS). “I feel that we are finally starting to recover from that slowdown.”
Cynthia Peterson highlights opportunities for growing CEUS' use in practice, including the modality's benefits toward patient care.
Despite the “modest” growth in CEUS’ clinical use, ultrasound imaging societies stay optimistic about the modality’s benefits. The AIUM Executive Committee supported ICUS’ initiative toward fair reimbursement for CEUS’ administration “in all its forms.”
“We believe [CEUS] and ultrasound more broadly will continue to grow as adoption expands across diagnostic and therapeutic applications,” AIUM president David Jones, MD, of the University of Vermont Medical Center in Burlington, told AuntMinnie. “It is essential that reimbursement policies keep pace with these advancements so patients can benefit from the innovations, improved outcomes, and the affordability of ultrasound compared to other imaging modalities.”
Peterson, meanwhile, said she hopes that the ultrasound community knows the value of CEUS in patient care.
“There are many developing applications and hopefully future approved indications that are going to be very beneficial to patients,” she said. “There is a learning curve, certainly for both physicians and sonographers, but a radiologist does not have to be in the room when this procedure is being performed.”