Microwave and radiofrequency ablation are safe and effective alternatives to surgery in older participants with hyperparathyroidism, according to a study published October 28 in Radiology.
The finding is from a trial of the procedures in 153 participants (mean age, 63), with high overall cure rates and few complications over a two-year follow-up period, noted lead author Luxin Zhang, MD, of the Medical School of the Chinese People’s Liberation Army in Beijing, and colleagues.
“This contrasts with the higher complication rates of parathyroidectomy in older adults, underscoring [microwave ablation, or MWA] and [radiofrequency ablation, or RFA] as a highly attractive option for patients who are frail or have contraindications for surgery,” the group wrote.
Primary hyperparathyroidism and secondary hyperparathyroidism are endocrine disorders that increase parathyroid hormone levels (PTH), which heightens the risk of osteoporosis and fractures and may lead to severe cardiovascular complications, the authors explained. While surgery is effective, parathyroidectomy is associated with risks such as respiratory complications, postoperative cardiovascular events, delirium, and phlebitis, particularly in older patients, they added.
Conversely, MWA and RFA are emerging minimally invasive ultrasound-guided procedures that can be performed under local anesthesia and result in minimal trauma, quick recovery, and few complications. So far, however, few studies of the techniques have included older participants, the researchers noted.
To bridge the gap, the group assessed outcomes among 153 patients over the age of 55 with primary hyperparathyroidism (PHPT) or secondary hyperparathyroidism (SHPT) who underwent microwave ablation or radiofrequency ablation at their hospital between September 2017 and March 2022.
For PHPT, the primary outcome was cure rate, defined as the proportion of participants who maintained normal PTH serum and calcium levels for at least six months. For SHPT, the primary outcome was defined as the proportion of participants who maintained PTH less than 585 ng/L for at least six months. Treatment-related complications were evaluated over a 24-month follow-up period.
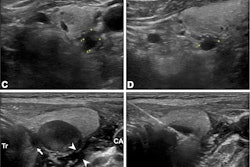
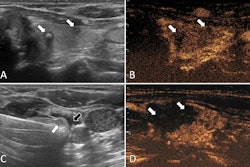
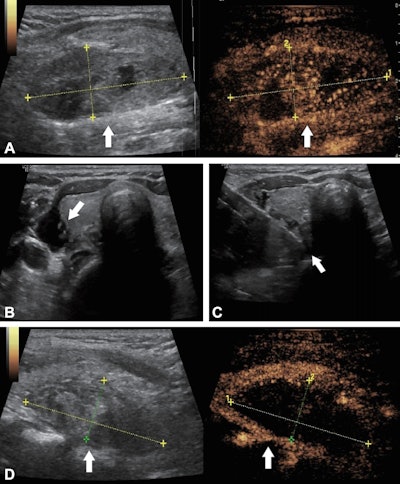 Ultrasound images in a 56-year-old woman with primary hyperparathyroidism treated using ultrasound-guided microwave ablation. (A) Preablation longitudinal images reveal a hypoechoic parathyroid nodule (arrow) measuring 4.84 × 1.86 × 2.53 cm. The B-mode image (left) shows the nodule, while the contrast-enhanced image (right) demonstrates hyperenhancement of the solid component of the parathyroid lesion. The coordinate axes indicate the measured maximum diameters of the nodule. (B) Transverse image shows percutaneous injection of saline solution (arrow) with ultrasound guidance, to create an isolation zone to protect surrounding tissues. (C) Transverse image shows the ablation needle (arrow) positioned within the nodule for microwave ablation. (D) Postablation longitudinal images of the lesion area (arrow). The B-mode image (left) shows the hyperechoic lesion area, while the contrast-enhanced image (right) shows no contrast enhancement, indicating complete ablation. The coordinate axes indicate the maximum diameters of the ablation zone (4.51 × 1.85 × 2.04 cm).RSNA
Ultrasound images in a 56-year-old woman with primary hyperparathyroidism treated using ultrasound-guided microwave ablation. (A) Preablation longitudinal images reveal a hypoechoic parathyroid nodule (arrow) measuring 4.84 × 1.86 × 2.53 cm. The B-mode image (left) shows the nodule, while the contrast-enhanced image (right) demonstrates hyperenhancement of the solid component of the parathyroid lesion. The coordinate axes indicate the measured maximum diameters of the nodule. (B) Transverse image shows percutaneous injection of saline solution (arrow) with ultrasound guidance, to create an isolation zone to protect surrounding tissues. (C) Transverse image shows the ablation needle (arrow) positioned within the nodule for microwave ablation. (D) Postablation longitudinal images of the lesion area (arrow). The B-mode image (left) shows the hyperechoic lesion area, while the contrast-enhanced image (right) shows no contrast enhancement, indicating complete ablation. The coordinate axes indicate the maximum diameters of the ablation zone (4.51 × 1.85 × 2.04 cm).RSNA
In addition, complications were minimal and transient, and preprocedure PTH level was an independent predictor of treatment failure in both participants with PHPT (odds ratio, 1.01; p = 0.02) and participants with SHPT (odds ratio, 1; p = 0.02).
“Thermal ablation has long been proposed as a minimally invasive alternative for patients who are poor candidates for parathyroidectomy, yet evidence in older cohorts has remained fragmentary,” the group wrote.
The researchers noted that the limited sample size of participants may have affected the precision of the findings and concluded that larger-scale randomized controlled trials that incorporate more comprehensive assessment parameters are warranted.
The full study is available here.