An MRI technique called quantitative susceptibility mapping (QSM) can predict the onset of mild cognitive impairment and cognitive decline in as-yet unimpaired older adults, researchers have reported.
The findings could lead to earlier interventions, according to a team led by senior author Xu Li, PhD, of Johns Hopkins University in Baltimore. The group's findings were published September 9 in Radiology.
"QSM is an advanced MRI technique developed over the last decade to measure tissue magnetic susceptibility with good precision," Li said in a statement released by the RSNA. "[It] can detect small differences in iron levels across different brain regions, providing a reliable and non-invasive way to map and quantify iron in patients, which is not possible with conventional MR approaches."
Alzheimer's disease consists of an accumulation of abnormal proteins in the brain, a condition that can appear years prior to clinical symptoms and can be detected with PET imaging. But previous research has also investigated the effect of elevated iron levels in the brain, noting that this overload can drive "neurodegeneration by inducing oxidative stress, exacerbating amyloid toxicity, disrupting tau protein function and promoting nerve cell death," the team wrote.
Li and colleagues conducted a study that included 158 cognitively unimpaired participants who participated in the Johns Hopkins Biomarkers for Older Controls at Risk for Dementia (BIOCARD) Study, a research project regarding the early stages of Alzheimer's disease. Of the study cohort, 110 had undergone PET imaging; all participants underwent QSM MRI for a baseline exam and then were followed for up to seven and a half years.
Overall, the investigators found that "higher baseline magnetic susceptibility on MRI in the entorhinal cortex and putamen -- two brain regions important to memory and other cognitive functions -- was associated with a higher risk of mild cognitive impairment, a transitional stage preceding Alzheimer's disease-related dementia."
"Using QSM, we found higher brain iron in some memory-related regions that are linked to a higher risk of developing cognitive impairment and faster cognitive decline," Li said. "This risk is even higher when the participants have higher levels of amyloid pathologies."
In fact, even though amyloid burden and tissue susceptibility in the entorhinal cortex and putamen were independently associated with progression to mild cognitive impairment, they appeared to have synergistic effects, the team wrote.
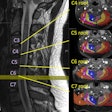
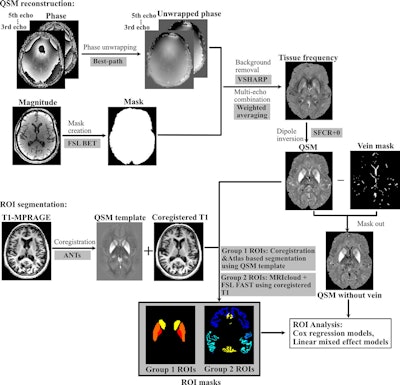 Processing pipeline for quantitative susceptibility mapping (QSM) reconstruction and region-of-interest (ROI) segmentation MRICloud is cloud-based medical image processing software (mricloud.org). ANT = advanced normalization tool, BET = brain extraction tool, FAST = functional MRI of the brain automated segmentation tool, FSL = functional MRI of the brain software library, MPRAGE = magnetization-prepared rapid gradient-echo, SFCR+0 = structural feature–based collaborative reconstruction with auto-referencing to central cerebrospinal fluid, VSHARP = variable radius sophisticated harmonic artifact reduction for phase data.Images and caption courtesy of the RSNA.
Processing pipeline for quantitative susceptibility mapping (QSM) reconstruction and region-of-interest (ROI) segmentation MRICloud is cloud-based medical image processing software (mricloud.org). ANT = advanced normalization tool, BET = brain extraction tool, FAST = functional MRI of the brain automated segmentation tool, FSL = functional MRI of the brain software library, MPRAGE = magnetization-prepared rapid gradient-echo, SFCR+0 = structural feature–based collaborative reconstruction with auto-referencing to central cerebrospinal fluid, VSHARP = variable radius sophisticated harmonic artifact reduction for phase data.Images and caption courtesy of the RSNA.
The study highlights the role QSM MRI could play in the workup of patients at risk of dementia, Li concluded.
"We can use this kind of tool to help identify patients at higher risk of developing Alzheimer’s disease and potentially guide early interventions as new treatments become available," he said. "Also, besides serving as a biomarker, brain iron may become a future therapeutic target."
This work is a "notable contribution to the growing body of imaging literature focused on preclinical detection of neurodegenerative conditions," according to an accompanying editorial by Carlota Andreu-Arasa, MD, PhD, of Boston University.
"As radiology increasingly intersects with molecular diagnostics and cognitive assessment, QSM may offer a noninvasive tool for risk stratification to guide individualized therapeutic strategies and care planning before the onset of symptoms," Andreu-Arasa wrote.
The complete study can be found here.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)