MRI and CT findings correlate for characterizing both the volume and quality of epicardial adipose tissue (EAT), according to a study published August 14 in Radiology: Cardiothoracic Imaging.
The findings are important because increased volume of epicardial adipose tissue has been linked to cardiovascular disorders, including coronary artery disease (CAD) and atrial fibrillation -- and both MRI and CT are used to characterize the tissue, noted a team led by Marjan Firouznia, PhD, of Linköping University in Sweden.
"EAT plays a dual role in cardiac health, providing energy substrates to the myocardium while also exerting harmful effects through proinflammatory and profibrotic cytokines," the group explained.
Epicardial adipose tissue can be analyzed via echocardiography, which measures its thickness but can't provide volumetric assessment, according to the researchers. CT and MR imaging quantify EAT volume with high spatial resolution, with the two modalities providing slightly different information (lower epicardial adipose tissue CT attenuation is associated with diabetes, CAD and increased risk of hospitalization for heart failure, while MRI helps characterize tissue fat content through quantifying fat signal fraction -- a technique used to characterize the liver and abdominal fatty tissue).
However, there's not much research that compares MRI's and CT's fatty tissue assessments, resulting in a "knowledge gap in the relationship between MRI and CT measurements of EAT," the researchers wrote. To address this gap, they conducted a study that included 92 patients who underwent MRI and CT between November 2017 and July 2018; data were culled from a subset of the Swedish CArdioPulmonary bioImage Study (SCAPIS).
Radiologist readers manually segmented Dixon fat-water separation MR images, using a fat signal fraction map to determine epicardial adipose tissue volume. Within this tissue volume, the readers quantified mean fat signal fraction as a measure of fat quality. As for CT, the readers used deep learning to segment EAT from CT images and to quantify its volume and mean attenuation. Finally, the investigators assessed any correlations between MRI- and CT-based measurements of epicardial adipose tissue volume and quality using the Pearson correlation coefficient (r).
Firouznia and colleagues reported the following:
- Correlation between MRI and CT results for EAT volume was very strong (r = 0.92, p < 0.001), but with "systematically larger values" for CT versus MRI (p < 0.001).
- There was a strong negative correlation between MRI fat signal fraction and CT attenuation (r = -0.72, p < 0.001) -- a finding that suggests that "the variation in CT attenuation of EAT is to a large extent explained by relative fat content," the authors wrote.
- Findings for MRI epicardial adipose tissue volume showed good interreader agreement (intraclass correlation coefficient, 0.86) and excellent intrareader agreement (intraclass correlation coefficient, 0.96) -- data that "make reader bias unlikely to have any major influence on our results," they explained.
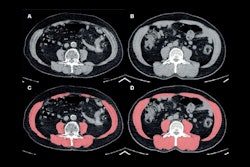
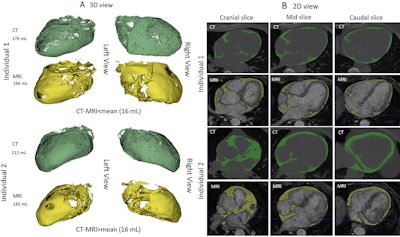 Images of epicardial adipose tissue segmentation in two male individuals with type 2 diabetes mellitus, aged 56 (individual 1) and 64 (individual 2) years, show volume differences less (upper two rows in A and B) or greater (lower two rows in A and B) than the mean volume difference of 16 mL between CT (in green) and MRI (in yellow). Deep learning was used for CT segmentation and semiautomated thresholding for MRI. (A) CT and MR images in the three-dimensional (3D) view. Both imaging modalities are presented from left and right views. (B) CT and MR images in the two-dimensional (2D) view. The stacked images consist of three selected 2D sections: cranial, mid, and caudal sections. All images are noncontrast images. Images and caption courtesy of the RSNA.
Images of epicardial adipose tissue segmentation in two male individuals with type 2 diabetes mellitus, aged 56 (individual 1) and 64 (individual 2) years, show volume differences less (upper two rows in A and B) or greater (lower two rows in A and B) than the mean volume difference of 16 mL between CT (in green) and MRI (in yellow). Deep learning was used for CT segmentation and semiautomated thresholding for MRI. (A) CT and MR images in the three-dimensional (3D) view. Both imaging modalities are presented from left and right views. (B) CT and MR images in the two-dimensional (2D) view. The stacked images consist of three selected 2D sections: cranial, mid, and caudal sections. All images are noncontrast images. Images and caption courtesy of the RSNA.
The study results suggest that EAT assessment can help both "predict and stratify cardiovascular risk in the clinical setting," the team noted, concluding that "assessment of [epicardial adipose tissue] volume has shown to add to the prediction of risk."
The complete study can be found here.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)