Multiparametric MRI's positive predictive value for detecting prostate cancer improves when lower apparent diffusion coefficient (ADC) values and patient prostate-specific antigen density (PSAD) thresholds data are incorporated, investigators have found.
The results could help further clarify mpMRI's benefits for this indication, noted a group of researchers led by Simon John Christoph Soerensen, MD, of Stanford University. The study findings were published August 12 in Radiology.
"Prostate multiparametric MRI (mpMRI) with MRI/ultrasound fusion biopsy improves the detection of clinically significant prostate cancer (csPCa) compared with systematic biopsy alone … and use of PI-RADS version 2.1 has reduced variability in acquisition, interpretation, and reporting," the investigators wrote.
What's tricky is that there tends to be a high false-positive rate from mpMRI for detecting prostate cancer, with positive predictive values (PPVs) of 35% for PI-RADS categories three or higher (i.e., intermediate or ambiguous likelihood of csPCa, high likelihood of the disease, to very high likelihood).
Adding data such as lesion apparent diffusion coefficient (ADC) value and patient prostate-specific antigen density (PSAD) could further refine PPVs, according to researchers. To assess the impact of these factors on mpMRI PPV for clinically significant prostate cancer across PI-RADs scores, they conducted a study that included 944 men with median prostate-specific antigen levels of 7 ng/mL and prostate volume of 46 cm3.
The study included data from 1,388 PI-RADS category 3 or higher lesions identified on mpMRI between January 2017 and December 2022, which were worked up via an MRI/ultrasound transrectal fusion biopsy within 180 days (median time from MRI to biopsy among the study cohort was 36 days). Twenty-two abdominal radiologists interpreted the mpMRI scans, with each reading at least 10 exams. Lesions were categorized as true positive if a genitourinary pathologist determined that targeted biopsy indicated a Gleason score grade group 2 or higher.
The group reported an overall lesion-level PPV for csPCa of 34%. PPV varied according to PI-RADS score:
| mpMRI performance for categorizing csPCa | |
| PI-RADS score | PPV |
| 3 | 11% |
| 4 | 33% |
| 5 | 59% |
When the team added ADC and PSAD data to mpMRI exam results, it found that low ADC and high PSAD were independent predictors of higher PPV (odds ratio, 3.52 and 3.35, respectively, with one as reference, p < 0.001). In fact, overall PPV increased from 12% for lesions with high ADC and low PSAD to 60% for those with low ADC and high PSAD, the group reported.
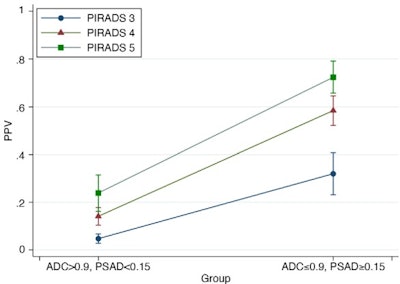 Graph shows the impact of dichotomized apparent diffusion coefficient (ADC) value and prostate-specific antigen density (PSAD) on positive predictive values (PPVs) across Prostate Imaging Reporting and Data System (PI-RADS) categories. In PI-RADS categories 3, 4, and 5, PPVs increased from 5% to 32%, 14% to 59%, and 24% to 73%, respectively, when comparing the group with ADC values of more than 0.9 × 10−3 mm2/sec and PSAD less than 0.15 ng/mL2 to that with ADC values of less than or equal to 0.9 × 10−3 mm2/sec and PSAD greater than or equal to 0.15 ng/mL2. The model represents estimates at a fixed lesion size of 1.2 cm, the median value of the study cohort. Figure and caption courtesy of the RSNA.
Graph shows the impact of dichotomized apparent diffusion coefficient (ADC) value and prostate-specific antigen density (PSAD) on positive predictive values (PPVs) across Prostate Imaging Reporting and Data System (PI-RADS) categories. In PI-RADS categories 3, 4, and 5, PPVs increased from 5% to 32%, 14% to 59%, and 24% to 73%, respectively, when comparing the group with ADC values of more than 0.9 × 10−3 mm2/sec and PSAD less than 0.15 ng/mL2 to that with ADC values of less than or equal to 0.9 × 10−3 mm2/sec and PSAD greater than or equal to 0.15 ng/mL2. The model represents estimates at a fixed lesion size of 1.2 cm, the median value of the study cohort. Figure and caption courtesy of the RSNA.
The study suggests that "incorporating lesion-level ADC values and patient PSAD thresholds substantially improves PPV at each PI-RADS category, suggesting a role for systematically adjusting lesion interpretation with these metrics," the investigators wrote.
They did caution, however, that the study did not analyze "potential decreases in sensitivity and in negative predictive value of mpMRI when incorporating ADC and PSAD thresholds," and urged these issues to be further evaluated in future studies intended to explore refinements of PIRADS guidelines.
The complete study can be found here.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











