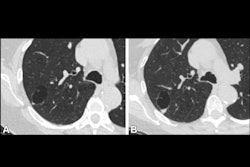
Incidental CT findings -- particularly on lung cancer screening (LCS) -- characterize interstitial lung abnormalities (ILAs) in Asian populations, researchers have reported.
The results address a knowledge disparity, as data regarding ILA-associated clinical outcomes such as lung cancer, idiopathic pulmonary fibrosis (IPF), and even mortality are scarce among Asians -- "despite potential differences in risk factors and disease patterns compared with Western populations," wrote a team led by Hyungjin Kim, MD, PhD, of Seoul National University Hospital in South Korea. The research was published May 27 in Radiology.
"In this context, the Korean National Lung Cancer Screening Program, implemented as a national cancer screening policy since 2019, provides a systematic population-based dataset that can be used to address these knowledge gaps and investigate the prevalence and clinical outcomes of ILAs in asymptomatic Asian individuals who smoke heavily," the investigators wrote.
Kim's group investigated the prevalence of ILAs and the association of ILAs with lung cancer, idiopathic pulmonary fibrosis (IPF), and mortality in a Korean cohort, including data from 125,600 individuals who participated in the Korean National Lung Cancer Screening Program between August 2019 and December 2020. The researchers identified ILAs from CT reports and assessed ILA prevalence across age groups. They also calculated incidence rate ratios for lung cancer, IPF, and all-cause mortality in patients with ILAs and those without.
The group found that patients with ILAs had a threefold higher risk of lung cancer (hazard ratio [HR], 3.18, with 1 as reference) and a twofold higher risk of all-cause mortality (HR, 2.37). Individuals with ILAS had a more than 60-fold higher risk of IPF diagnosis (HR, 63.4).
The team also reported the following:
- Overall ILA prevalence was 2.7% (3,324 of 125,600) and was associated with older age (p < 0.001).
- The lung cancer incidence rate was higher in the ILA group (2,009 vs. 412 per 100,000 person-years [p < 0.001; incidence rate ratio, 4.88, with 1 as reference]).
- The all-cause mortality rate was also higher in the ILA group (2,334 vs. 712 per 100,000 person-years [p < 0.001; incidence rate ratio, 3.28]).
- Over a median follow-up of 2.9 years, 3.5% of patients with ILAs were diagnosed with IPF for an incidence rate of 1,344 per 100,000 person-years vs. 18 per 100,000 person-years in individuals without ILAs (incidence rate ratio, 73.24; p < 0.001).
ILAs are "no longer regarded as incidental findings on images; instead they represent a clinically meaningful spectrum of early interstitial changes with implications for management and long-term outcomes," wrote Dhiraj Baruah, MD, and Ismail Mikdat Kabakus, MD, both of the Medical University of South Carolina, in an accompanying commentary.
"These findings reinforce that ILAs should be recognized as early markers of serious pulmonary disease processes, rather than being considered inconsequential imaging observations," they noted. "Early identification of ILAs may allow for timely intervention, risk stratification, and more personalized surveillance strategies, potentially altering disease progression and improving patient outcomes."
The complete study can be found here.