Radiologists are getting paid for about half of the software-as-a-service (SaaS) AI services they submit to Medicare, according to a study published September 11 in the Journal of the American College of Radiology.
Between 2018 and 2023, radiologists received $8 million in payments -- $4.6 million in 2023 alone -- but were denied a potential $16.4 million, according to corresponding author Joshua Liao, MD, of the University of Texas Southwestern Medical Center in Dallas, and colleagues.
“The rapid increase in, but only partial reimbursement for, AI services among radiologists in Medicare underscores structural and behavioral facilitators and barriers to diffusion of AI innovation,” the group wrote.
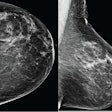
More than 1,200 AI-enabled medical devices have received regulatory approval in the U.S. since 2016, with about 81% of these being radiology-based. While prior studies have evaluated AI adoption among all physicians in commercially insured patients, none have evaluated adoption among radiologists specifically or adoption in Medicare, the authors explained.
To address the knowledge gap, the researchers delved into data on Medicare Part B carrier fee-for-service claims for SaaS-based AI services between 2018 and 2023. They used Current Procedural Terminology (CPT) codes to identify 23 services approved by Medicare for reimbursement through the Physician Fee Schedule at some point over the study period.
Overall, radiologists provided and submitted a total of 83,392 AI services, the researchers reported. Among these, 47.4% (n = 39,535) were accepted and reimbursed (reflecting $8 million in payments), while 52.6% (n = 43,857) of services were denied, which would have corresponded to $16.4 million in reimbursements.
In terms of service type, CT-derived fractional flow reserve (CPT code 0501T-0504T) had the greatest use, with 35,845 accepted services (90.7% of all accepted services), reflecting $7.8 million of reimbursements.
Over time, adoption increased from 1,507 services in 2018 to 53,586 services in 2023. Accepted services increased from 424 services (28.1%) in 2018, reflecting $30,000 in payments, to 17,014 services (31.8%) in 2023, reflecting $4.6 million in payments, according to the results.
In addition, denied AI services also increased across this period, from 1,083 services (71.9%) in 2018, reflecting $60,000 in potential payments, to 36,572 services (52.6%) in 2023, reflecting $10.2 million in potential payments.
Finally, the researchers noted that AI services were most commonly adopted in on-campus outpatient hospitals (24,254 accepted services, 61.3% of all accepted services), followed by physician offices (12,721 services, 32.2% of all accepted services). A minority of services were adopted in off-campus outpatient hospitals (1,365 services), inpatient hospitals (901 services), independent clinics (254 services), and emergency rooms (30 services).
The researchers noted that analysis of SaaS-based AI may not extrapolate to non-SaaS AI software as a medical device or AI software embedded in a medical device. Also, data limitations precluded them from identifying specific reasons for claims denials.
Ultimately, while the U.S. Centers for Medicare and Medicaid Services have expanded reimbursable SaaS-based AI over time, reimbursement policies have been incomplete and arguably fragmented due to reliance on a patchwork of national and local coverage determinations, the researchers wrote.
“Increasing AI adoption in Medicare provides empiric evidence for the need to design payment systems suitable for such services,” the group concluded.
The full study is available here.