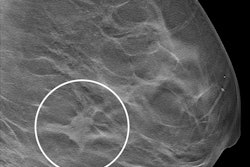
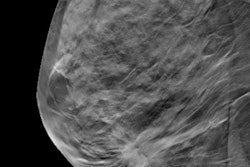
Digital breast tomosynthesis (DBT) plus synthesized mammography leads to lower false-positive recall rates versus digital mammography, suggest findings published September 16 in Radiology.
A team led by Stefanie Weigel, MD, from the University of Münster and University Hospital Münster in Germany reported that this finding especially went for first-round screening participants. And while this combined approach slightly raised false-positive biopsies, it also led to more detected breast cancers.
“The positive predictive value [PPV] of recall was consistently higher with DBT plus synthesized mammography,” the Weigel team wrote.
The TOmo-synthesis plus SYnthesized MAmmography (TOSYMA) trial was a randomized controlled trial involving about 100,000 participants that ran from 2018 to 2020. It confirmed significantly higher detection rates of invasive breast cancers with DBT plus synthesized mammography, a 48% difference compared with standard digital mammography.
Weigel and colleagues performed a subanalysis of the TOSYMA data, comparing screening with DBT plus synthesized mammography versus digital mammography in terms of false-positive recall and false-positive biopsy rates, as well as their PPVs. The subanalysis included 49,762 women in the digital mammography arm and 49,715 women in the combined approach arm.
The researchers found that DBT plus synthesized mammography led to a lower recall rate, a higher true-positive rate, and a lower false-positive recall rate.
Comparison in performance between breast cancer screening approaches | ||
Measure | Digital mammography | DBT plus synthesized mammography |
Recall rate (per 1,000 women) | 49.9 | 48.6 |
True-positive rate (per 1,000 women) | 6.2 | 8.4 |
False-positive recall rate (per 1,000 women) | 43.7 | 40.2 |
False-positive recall rate in first-round screening (per 1,000 women) | 109.6 | 94 |
PPV of recall | 12.3% | 17.2% |
The combined approach did lead to a higher false-positive biopsy rate (7.8 per 1,000 women screened) compared to digital mammography (6 per 1,000 women screened). The PPV of biopsies performed was 51.7%. It also led to slightly more benign surgical excisions (1.2 per 1,000 women screened) compared to digital mammography (0.6 per 1,000 women screened).
The team reported just five interval cancers after false-positive recalls for DBT plus synthesized mammography and two interval cancers for digital mammography.
The researchers suggested that the lower recall rate for first-time participants with the combined approach is due to a lower rate of false-positive recalls, with digital mammography having more summation shadows.
“In subsequent-round participants, such abnormalities are commonly less likely to be recalled because of comparisons with prior examinations, which reduces the differences in false-positive recalls between digital mammography and DBT plus synthesized mammography,” they wrote.
And while the combined approach led to “mildly” raised false-positive biopsies with DBT, this was “compensated with the detection of more breast cancers.”
The study results may persuade health leaders still hesitant to replace digital mammography with synthesized mammography alongside DBT, according to an accompanying editorial written by Benoît Mesurolle, MD, from Centre République in Clermont-Ferrand, France, and Mona El Khoury, MD, from Centre Hospitalier Universitaire de Montréal in Canada.
The duo wrote that this would reduce radiation exposure without compromising the effectiveness of screening with DBT.
“TOSYMA explores the use of DBT in population screening through a pragmatic, real-world study design,” they added. “Increasing evidence supports the use of DBT in screening settings.”
Read the full study here.