An AI-based breast cancer risk prediction model achieved high accuracy in a racially and ethnically diverse population in a study published June 6 in JAMA Network Open.
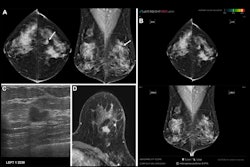
Researchers led by Shu Jiang, PhD, from Washington University in St. Louis, MO, reported that their AI model, which generated mammogram risk scores from both current and prior mammograms, performed well across diverse racial and ethnic populations in a province-wide screening program starting at age 40.
“The dynamic risk prediction model used in this prognostic study makes full use of each woman’s own mammograms for personalized long-term risk prediction,” Jiang and co-authors wrote.
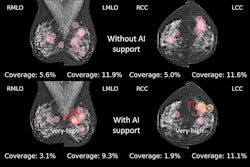
Researchers continue to explore AI’s potential in breast imaging, with studies showing the potential of AI tools serving in an adjunct role. However, one challenge that persists is how these tools can be generalizable across diverse populations, considering that breast cancer is not a one-size-fits-all disease.
Jiang and colleagues tested the performance of their dynamic risk prediction model incorporating prior mammograms, which was previously validated in Black and white women. They tested the model in a province-wide screening program in British Columbia, where mammographic breast screening starts at age 40 years and is provided every other year.
The final analysis included 206,929 women with an average age of 56.1 years. Of the total, 118,093 women had reported data on race. This included 34,266 East Asian women, 1,946 women who reported as Indigenous, 6,116 South Asian women, and 66,742 white women. The team found 4,168 pathology-confirmed incident breast cancers diagnosed, with an average follow-up time of 5.3 years.
Using up to four years of prior mammograms in addition to the most current mammograms, the model achieved an area under the receiver operating curve (AUROC) of 0.78 based on analyzing images alone. It also achieved consistent results throughout the study’s subpopulations. This included the following AUROC values: 0.77 in East Asian women, 0.77 for Indigenous women, and 0.75 for South Asian women.
When stratified by age, the model achieved AUROC values of 0.76 for women ages 50 or younger and 0.8 for women older than 50.
Finally, the team reported 18,839 women with a five-year risk greater than 3%, including a positive predictive value of 4.9% and an incidence of 11.8 per 1,000 person-years.
The study authors wrote that, along with the mammogram risk score’s accuracy, the model could help improve the use of resources in breast cancer screening by making risk assessment more feasible and accessible.
“Given the global burden of breast cancer among women, and the range of screening intervals and starting ages in screening programs, it is imperative to use existing image data to more accurately assess risk to guide precision prevention and maximize population benefits,” they wrote.
The full study can be found here.