Breast cancer status and exam indication should be factored into axillary ultrasound interpretation, according to research presented May 1 at the American Roentgen Ray Society (ARRS) annual meeting in San Diego, CA.
In his talk, Howard Yan, MD, from Stanford Health Care in California, discussed his team’s findings, showing that about three out of every five axillary ultrasound exams are performed on women without breast cancer, with a low rate of lymph node metastases. The group also reported that clinical concern was the most common indication, while treatment planning was the least common one.
“The one-size-fits-all approach that’s currently used in our setting, and I’m sure used in many other institutions, should really be called into question,” Yan said.
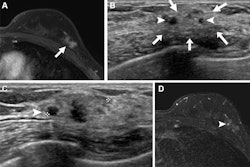
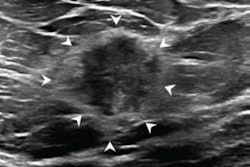
Axillary ultrasound is used in various clinical situations. These could include axillary lumps in women with no breast cancer history, axillary staging for newly diagnosed cancers, or suspicious axillary lymph nodes seen on other imaging modalities, for example.
However, Yan noted that the same set of criteria is often used for these situations, being derived from existing literature on the breast cancer population.
“In the clinical setting, we see that the outcomes differ significantly,” Yan said.
He and colleagues investigated how indication and breast cancer status affect the prevalence of lymph node metastases, axillary ultrasound exam performance indices, and features of lymph node metastases on ultrasound.
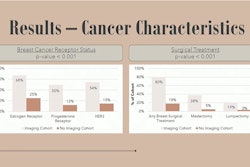
The study included data collected between 2017 and 2020 from 2,156 axillary ultrasound exams in 1,719 women. Of the total women, 135 (6.3%) had lymph node metastasis.
Women without breast cancer receive the majority of ultrasound exams at 62.2% (n = 1,340), with a cancer prevalence of 1.7% (n = 23 of 1,340). Meanwhile, women with current breast cancer made up 12% of axillary ultrasound exams in the study population (n = 70 of 259), with a prevalence of 27%.
Also, clinical concern was the most common indication at 49.4% (n = 1,064), with a cancer prevalence of 3.1%. Treatment planning, meanwhile, was the least common indication at 5% (n = 108), with a prevalence of 24.1%. Follow-up and routine evaluation had a combined prevalence of 0.2%.
Finally, Yan reported that lymph node metastases in women without current breast cancer had larger cortices and were more likely to have absent hilum and abnormal shape.
With these results in mind, he highlighted that axillary ultrasound should only be performed when indicated. This includes having conversations about raising or lowering the abnormal threshold for biopsy and stop assigning lymph nodes as “probably benign” outside of vaccine-related cases. He added that indication and breast cancer status should be considered when axillary ultrasound is performed on this population.
“These [outcomes] are readily available at the time of interpretation, and I think we should look into that very carefully and make decisions accordingly based on the images and these two factors,” he said.