In-hospital triage protocols, rapid staff mobilization, and versatile imaging resources management are critical for radiology department when responding to mass casualty incidents (MCIs), according to a study published September 30 in Radiology.
In an interview with AuntMinnie.com, lead author Gal Ben-Arie, MD, of Soroka University Medical Center in Be’er-Sheva, Israel, discussed the unique lessons learned at the hospital on October 7, 2023, when armed Hamas militants breached the security fences along the Israel-Gaza border and launched a coordinated attack.
“In most MCIs, there is a single event that takes place and then patients flow into the hospitals during a certain time ... We had casualties arriving to the hospital for a long duration. The chaotic phase of the MCI was very, very long,” he explained.
In all, a total of 461 patients underwent imaging during the crisis, with 400 patients arriving within the first eight hours of the attack, Arie and colleagues reported. Digital radiography was performed in 351 patients and CT was performed in 164 patients; 54 patients underwent imaging with both modalities.
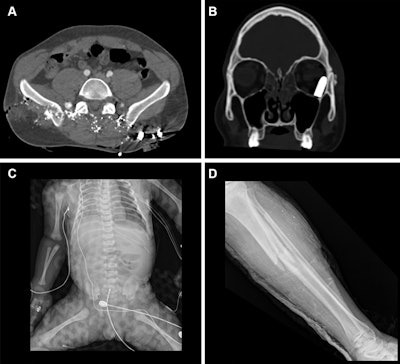 Representative injuries in patients from the mass casualty incident of October 7, 2023. (A) Axial CT scan at the pelvic level in a 34-year-old male patient shows multiple shrapnel fragments in the pelvis, resulting in fractures of the pelvic bones and lumbar vertebrae (not visible on this image). (B) Coronal reconstruction of a head CT scan in a 20-year-old male patient shows penetrating trauma to the left eyeball with a retained bullet in the orbital cavity. (C) Radiograph of a fetus delivered by emergency cesarean section
Representative injuries in patients from the mass casualty incident of October 7, 2023. (A) Axial CT scan at the pelvic level in a 34-year-old male patient shows multiple shrapnel fragments in the pelvis, resulting in fractures of the pelvic bones and lumbar vertebrae (not visible on this image). (B) Coronal reconstruction of a head CT scan in a 20-year-old male patient shows penetrating trauma to the left eyeball with a retained bullet in the orbital cavity. (C) Radiograph of a fetus delivered by emergency cesarean section
from a critically injured mother shows a left pneumothorax and catheter in place. (D) Radiograph in a 25-year-old female patient shows a comminuted fracture in the tibial metaphysis with fragment displacement and multiple bony fragments in the surrounding soft tissues.RSNA
“The October 7, 2023, MCI at SUMC provided a framework for evaluating the ability of the radiology department to be prepared for and to adapt to extreme conditions, offering generalizable strategies that may be implemented in other disastrous situations,” the group concluded.
The full study is available here.