SINGAPORE – A machine-learning model using radiomics features from MRIs could help clinicians predict whether patients with knee osteoarthritis may need total knee replacement (TKR) surgery.
In a study discussed May 5 at the annual meeting of the International Society for Magnetic Resonance in Medicine (ISMRM), a model distinguished knee osteoarthritis patients in potential need of TKR with an accuracy of up to 87.2%.
“These advancements have the potential to help the precision of decision-making in TKR surgery,” noted presenter Eros Montin, PhD, of New York University in New York City.
Knee osteoarthritis affects millions worldwide, with TKR a common treatment for individuals with advanced disease. MRI exams can diagnose knee osteoarthritis and track its progression, based on changes in the knee’s cartilage and meniscus.
Radiomics is a quantitative approach that extracts high-throughput features invisible to the eye from MRI scans for computational predictions, Montin explained. In this research, he and colleagues used such features to build a model that predicts osteoarthritis progression and treatment outcomes.
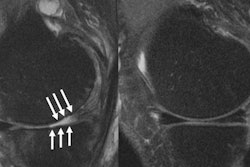
 In the figure it is possible to see the images and ROIs used in this study: images were acquired using a sagittal intermediate-weighted turbo spin echo (TE = 30 ms, TR = 3,200 ms, FOV = 160 mm, Slice Thickness = 3 mm, In-plane Resolution = 0.36 mm × 0.51 mm, Bandwidth = 248 Hz/pixel, Matrix Size = 444 × 448 × 37). In yellow, the femoral cartilage, in brown, the patellar cartilage, in red, the medial meniscus, in green, the lateral TBL Cartilage, in blue, the medial TBL Cartilage, and in purple, the lateral meniscus. Image courtesy of Eros Montin, PhD.
In the figure it is possible to see the images and ROIs used in this study: images were acquired using a sagittal intermediate-weighted turbo spin echo (TE = 30 ms, TR = 3,200 ms, FOV = 160 mm, Slice Thickness = 3 mm, In-plane Resolution = 0.36 mm × 0.51 mm, Bandwidth = 248 Hz/pixel, Matrix Size = 444 × 448 × 37). In yellow, the femoral cartilage, in brown, the patellar cartilage, in red, the medial meniscus, in green, the lateral TBL Cartilage, in blue, the medial TBL Cartilage, and in purple, the lateral meniscus. Image courtesy of Eros Montin, PhD.
First, the group used a pretrained deep learning-based algorithm to segment the articular (femoral, tibial, and patellar) cartilage and meniscus in MRI images from 143 patients who had undergone surgery within nine years from their baseline measurement. This resulted in the identification of six regions of interest (ROIs).
Next, they extracted a total of 10,494 radiomics features from the MRI images for each subject and further identified the four most relevant features in each ROI to add to the model.
To test the model, the group assessed its accuracy on MRIs from a matched control group also comprising 143 individuals who also underwent TKR, yet not within the same time frame (within nine years from baseline).
According to the analysis, the model correctly classified patients as being in need of TKR with an accuracy of 87.2% and a precision (true positives) of 89.1%. Montin noted that the model was not as good at identifying true negatives, however.
“Interestingly, three out of the four most significant radiomic features selected … were all derived from the meniscus areas, suggesting that the meniscus may play a crucial role in predicting patient outcomes,” he noted.
Ultimately, further research is warranted to improve the model’s ability to identify true negatives and to validate its performance in larger and more diverse patient population, Montin concluded.