Ending out-of-pocket patient payments for digital breast tomosynthesis (DBT) can increase overall utilization for breast cancer screening, but it doesn’t completely eliminate racial disparities, according to a study published June 19 in the Journal of the American College of Radiology.
Nonetheless, the research shows that eliminating these types of payments can be an effective approach to effectively aid in facilitating adoption of new technologies, according to researchers led by Nina Capiro, MD, of the University of California, Los Angeles,
“More work needs to be done to bring parity to screening mammography among patients, as this will ultimately contribute to reducing disparities in breast cancer outcomes across patient groups,” Capiro and colleagues wrote.
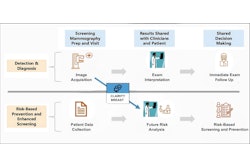
DBT received U.S. Food and Drug Administration (FDA) clearance in 2011, but many insurers didn’t immediately adopt full coverage of the procedure without patient cost sharing. A $45 out-of-pocket fee had initially been charged at the group’s academic institution and affiliated outpatient imaging centers, but was refunded after insurance payment was received. After most insurers began covering DBT, this fee was eliminated in January 2021.
To assess the effect of out-of-pocket costs on the use of DBT vs. digital mammography for breast cancer screening across different patient groups, the researchers retrospectively analyzed screening mammograms conducted before (March 2018 to January 2021) and after (February 2021 to August 2022).
Overall DBT utilization increased from between 11,123 and 13,284 (83.7%) to between 12,256 and 13,284 (91.5%) after the out-of-pocket cost was eliminated.
Relative to white patients, DBT utilization increased by 6.2 percentage points for Hispanic patients, by 6.2 percentage points for Black patients, and by 5.2 percentage points for Asian patients.
In other findings, DBT utilization climbed for non-English-speaking patients by 7.1 percentage points more than English speakers. Furthermore, the researchers calculated that Medicaid and commercially insured patients had a higher increase in DBT usage (7.1 percentage points and 6.7 percentage points, respectively) than Medicare patients.
It's important to note, however, that these disparities were not completely eliminated, according to the researchers.
“Even following the removal of the fee for screening DBT, White patients, English-speaking patients, patients with Medicare and those from less socioeconomically vulnerable areas continued to have the highest rates of DBT utilization when compared to other groups," the authors wrote. "These persistent differences may result from other systemic factors, such as physician referral patterns, patient health literacy, or lingering concerns about healthcare costs. Addressing these remaining barriers should be a priority for future interventions to further advance equity in breast cancer screening.”
The full article can be found here.