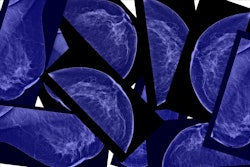
AI can accurately predict cardiovascular (CV) risk by analyzing mammograms, according to results published September 16 in Heart.
Researchers led by Clare Arnott, PhD, from the George Institute for Global Health in Sydney, New South Wales, Australia, developed a deep-learning algorithm based on only mammographic features and age to predict CV risk. They reported that the algorithm was on par with traditional cardiovascular risk equations.
“We have potentially identified a two-for-one screening test. The hope is that we can integrate this into breast screen centers in an automated fashion,” Arnott told AuntMinnie. “Women identified as moderate or high risk can then be prompted to see their primary care physician for a CV risk assessment.”
Previous studies point to breast arterial calcification (BAC) being tied to higher CV risk in women. These calcifications are also linked to vascular risk factors such as diabetes, hypertension, and hypercholesterolemia. Other mammographic features, including microcalcifications and breast density, may also be associated with cardiometabolic disease risk and mortality.
The researchers developed and internally validated an algorithm that predicts CV risk in women attending routine screening mammography for breast cancer. They developed the prediction model by using the DeepSurv architecture to compile radiomics data from mammograms and patient age.
The study included data from 49,196 women with no evidence of prior CV disease, an average age of 59.6 at baseline, and a median follow-up of 8.8 years. Of the total women, 3,392 experienced a first major CV event.
The DeepSurv model using mammography features and patient age had a concordance index of 0.72. To compare, the American Heart Association’s “Prevent” equations led to concordance indices of 0.76 (for men) and 0.79 for women; New Zealand’s “Predict” model had an index of 0.73. The latter two models use age and clinical variables in their respective prediction risk assessments.
Finally, the team’s combined model that used clinical characteristics and radiomic data achieved a concordance index of 0.75.
Arnott said that the model can be integrated into routine breast cancer screening without interrupting mammography services.
“There is a huge body of work from us as clinicians and public health advocates to encourage women to use this screening,” she said.
Arnott also told AuntMinnie that the team is performing qualitative research with breast screening organizations, women, and general practitioners to understand barriers and facilitators to implementation.
“Following this, we will conduct an implementation trial in breast screen services nationally [in Australia],” she added. “In addition, we are working with overseas collaborators on external validation of the algorithm in other populations.”
Read the full study here.