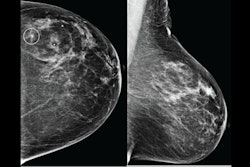
AI may be able to replace second readers in double-reading settings for breast cancer screening, suggest findings published August 14 in The Lancet Digital Health.
Researchers led by Ritse Mann, MD, PhD, from the Radboud University Medical Center in Nijmegen, the Netherlands, found that evaluating screening mammograms with one human reader and AI led to more cancers being found than conventional double reading, regardless of breast density.
“I really think it’s important to get AI into practice, and we should be aware of the potential of AI to help with our eventual goal, which is reducing mortality from breast cancer,” Mann told AuntMinnie. “And that’s a real possibility nowadays.”
Researchers continue to develop AI systems that can automate the evaluation of screening mammograms with performances comparable to those of radiologists. The investigators highlighted that successful AI integration into breast imaging settings could provide relief for practices that struggle with employee shortages, adding that AI one day may improve screening outcomes by faster reading time and greater accuracy.
In its retrospective study, Mann's team evaluated the performance of population-based breast cancer screening when using a commercially available system (Transpara v.1.7.0, ScreenPoint Medical) as an independent or second reader. They tested the AI’s performance on different screening situations.
The analysis included 42,236 consecutive 2D mammograms from 42,100 women from Dutch population-based screening data. After follow-up, 580 mammograms from 579 women were labeled positive. These included 291 screen-detected cancers, 102 interval cancers, and 187 future-detected breast cancers.
Ritse Mann, MD, PhD, further explains the results from a study he and colleagues led, showing AI’s potential as a second reader in breast cancer screening.
The researchers reported the following:
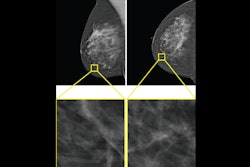
Conventional double reading led to 1,244 recalls (2.9%, 291 screen-detected cancers), while the reader plus AI approach recalled 2,112 mammograms. This improved the sensitivity by 8.4% (p < 0.0001).
Of the total recalled mammograms with the AI approach, 5% contained cancers. This included 282 screen-detected cancers, 29 interval cancers, and 38 future-detected breast cancers.
The team found no significant difference in performance in the one reader plus AI approach across breast density categories.
AI found future-detected breast cancers and interval cancers that were missed by the original human readers. These cancers were more often invasive (+26.7%) and/or had tumors greater than 20 mm (+16.6%) by the time they were found compared with the average screen-detected cancers.
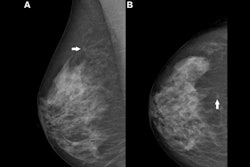
Finally, about two-thirds of screen-detected cancers (194 of 291) involved invasive breast cancer. Of the cancers found by AI, 71% (157 of 221) of recognized screen-detected cancers and 93.4% (57 of 61) of recognized invasive cancers and future-detected breast cancers were invasive at their eventual finding.
The study authors highlighted that AI finding cancers at low recall rates shows the potential of these cancers being detectable at an earlier time. The results also suggest that commonly reported program sensitivities “provide an overly optimistic view on the detection capability of mammographic screening.”
Mann discusses the implications of the study on AI's inevitable role in breast care.
The authors added that since interval cancers and future detected breast cancers are later found through screening or due to clinical presentation, “this does not increase overdiagnosis.”
However, they called for an effective arbitration process for human and AI-recalled cases.
"Extended research with diverse AI systems and datasets, including more comprehensive long-term follow-up, is required," the authors concluded.
The full study can be found here.