How best can photon-counting CT (PCCT) resources be allocated? There are a number of ways to tackle the problem, including creating a department review board, according to a September 4 talk delivered at the International Society of Computed Tomography (ISCT) symposium in Brussels.
Clinically, PCCT is a valuable form of CT imaging when it comes to spatial resolution, dose reduction potential, increased contrast resolution, and multienergy imaging, but for most practices, the technology is a scarce resource, explained Adam Froemming, MD, professor of radiology at the Mayo Clinic in Rochester, MN.
"[We] can think of many clinical applications that benefit from at least one, if not more than one of [PCCT's] features, which makes it valuable," he said. But he also underscored some of the operational challenges and strategies for managing PCCT in a conventional energy-integrating detector (EID) CT environment.
Froemming is an abdominal radiologist. He serves as chair of CT imaging at Mayo and has a vested interest himself among competing interests, such as cardiac imaging. If a department's abdominal practice is 50% of all CT volume, should it get 50% of the access on this photon-counting scanner? Should clinical divisions get equal timeshare? There's much to consider, Froemming explained.
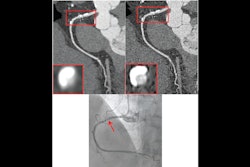
"We had a policy that you had to convince the group," he said, noting examples where the group saw evidence that diagnostic imaging using PCCT improved patient management and outcome in cases involving temporal bone imaging (highlighting an eroding ossicular implant), and pediatric cystic fibrosis.
"Those are both diagnoses that were only able to be made on this scanner that could not be made when the patient was scanned on the conventional force scanner," Froemming said, noting "huge dose reduction potential, and much more actionable clinical information."
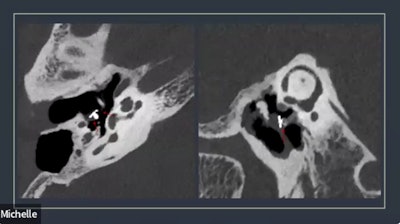 Temporal bone imaging using photon counting CT illuminated the ossicular implant.Adam Froemming, MD, Mayo Clinic, via ISCT.
Temporal bone imaging using photon counting CT illuminated the ossicular implant.Adam Froemming, MD, Mayo Clinic, via ISCT.
Froemming also recognized literature that supports the value of PCCT for cardiovascular applications, and stressed that it is important to allocate resources where PCCT leaves "no operational white space."
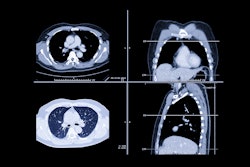
Mayo placed PCCT in a high-throughput outpatient location that scans patients from early in the morning until late at night and serves the bulk of their thoracic outpatient practice. The hospital also positioned it for CT technologist training, which Froemming said was a significant struggle in the beginning.
During the talk, he acknowledged that CT technologist training was difficult due to established practices and said, "If you are going to have one [scanner], you could consider saying, 'I only need two or three really highly trained techs to run it.' If you think your fleet is going to be 50% of these scanners in the next five years, you have to have your whole fleet of technologists trained."
Other operational challenges include the scanner's sensitivity to room temperature changes, humidity changes, and the temperature of the cold-water line. "That was all much more significant than we had thought coming into it," Froemming said.
In addition, he said PCCT scanners produce exams that are four times more image-dense and data-dense than conventional scans -- making it crucial to establish an IT infrastructure to support radiologists.
Mayo's Rochester campus operates four main fleets of CT scanners, according to Froemming. The PCCT resource allocation review board consists of CT experts from the different clinical domains, such as pediatrics, the emergency department, thoracic imaging, abdominal, musculoskeletal, and cardiovascular, and includes the physicist.
"In your system, you have to figure out how to operationalize getting high-priority patients directed specifically to that [PCCT] machine," he concluded. "With a lot of competing demands to sort out, a different set of processes is also needed to prevent activities that are not clearly beneficial to the practice."